Abstract

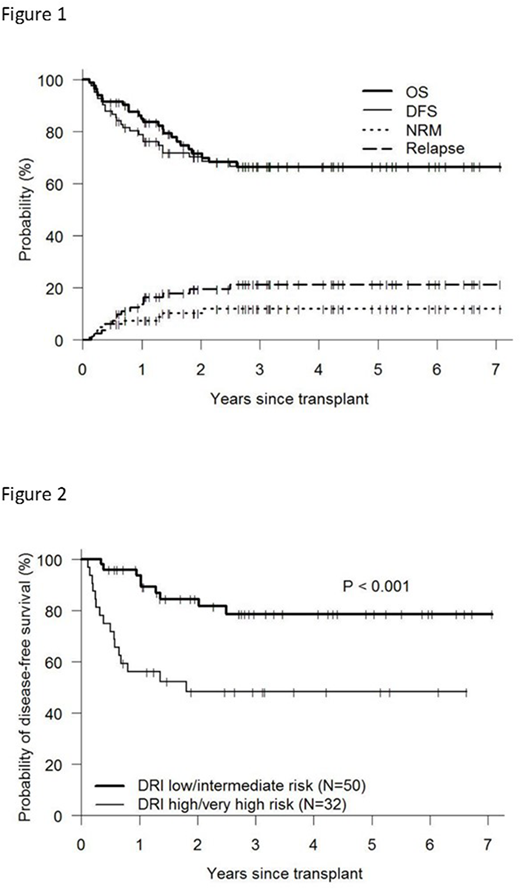
Haploidentical donor (HID) transplant with post-transplant cyclophosphamide (PTCy) is being increasingly utilized worldwide. Although the original "Baltimore" protocol employed nonmyeloablative conditioning, there has been increasing interest in the use of myeloablative conditioning (MAC) in an attempt to decrease the risk of disease recurrence and graft failure. We present the long-term follow-up results of 82 consecutive patients receiving a MAC HID transplant at a single institution between 2011-2017, following a uniform protocol of Fludarabine/total body irradiation (TBI) 1200cGy conditioning, PTCy, tacrolimus and mycophenolate mofetil. PBSC was utilized as the graft source for all transplants and graft CD34 dose was capped at 5 x 106/kg. Median patient age was 42 (range 19-61) years. The most common diagnoses were AML (51%) and ALL (33%), and 39% were high/very high disease risk index (DRI). Donor was a child, sibling or parent in 35%, 43% and 22% respectively. Median follow-up time for surviving patients was 37 months. Primary engraftment occurred in all patients, with all patients achieving complete donor T cell and myeloid chimerism by day +30. There were no cases of late graft failure. The cumulative incidence of grade 3-4 acute graft-versus-host disease (GVHD) and moderate-to-severe chronic GVHD was 17% and 22%, respectively. Non-relapse mortality (NRM) was 7% at one year and 12% at three years post-transplant. Overall survival at 1, 2, and 3 years post-transplant was 85%, 72% and 66% respectively (figure 1). Estimated 3-year DFS, current GVHD-, relapse-free survival (CGRFS), conventional GRFS, and relapse was 67%, 62%, 43%, and 21% respectively. DFS at 3-yr was significantly improved in patients with low/intermediate vs high/very high DRI (79% vs. 48%, figure 2) due to a lower risk of relapse (12% vs. 36%). Infectious complications included CMV reactivation in 55% of patients (CMV disease - 2%) and BK virus infection in 38% (severe - 2%). There were no reported cases of EBV lymphoproliferative disease. This large single institution analysis with long-term follow-up confirms the feasibility of Fludarabine/TBI-based MAC HID transplant with PBSC/PTCy in younger adult patients. This is supported by both the high rate of engraftment, low NRM and a 3-yr CGRFS of 62% (suggesting freedom from relapse and need for long-term systemic immunosuppression for GVHD). The achievement of long term DFS in approximately 80% of low/intermediate DRI and half of high/very high DRI patients is promising.
Solh:ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal